Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

HOST-PARASITE INTERACTIONS IN PERIODONTAL DISEASE •
1
53
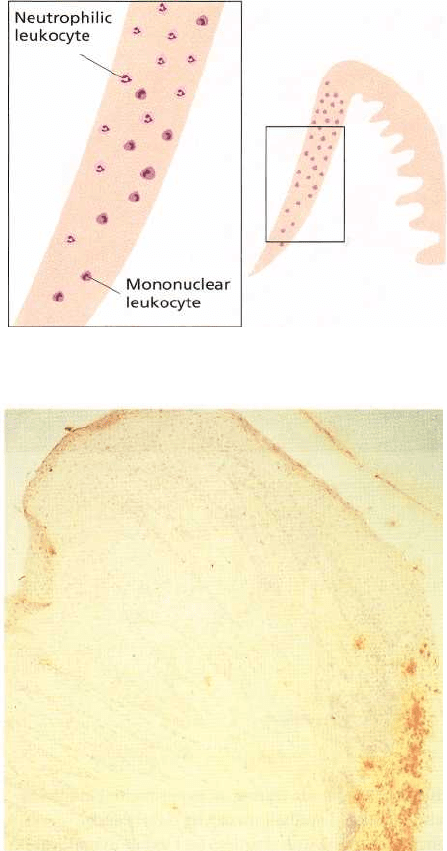
Fig. 5-3. Leukocytes in the junctional epithelium. Ob-
serve that the volume of leukocytes decreases in apical
direction and approaches 0 in the most apical portion.
Within the junctional epithelium, the mononuclear leu
kocytes are located in more basal layers, while the
neutrophilic granulocytes are present primarily in the
superficial portions of the junctional epithelium.
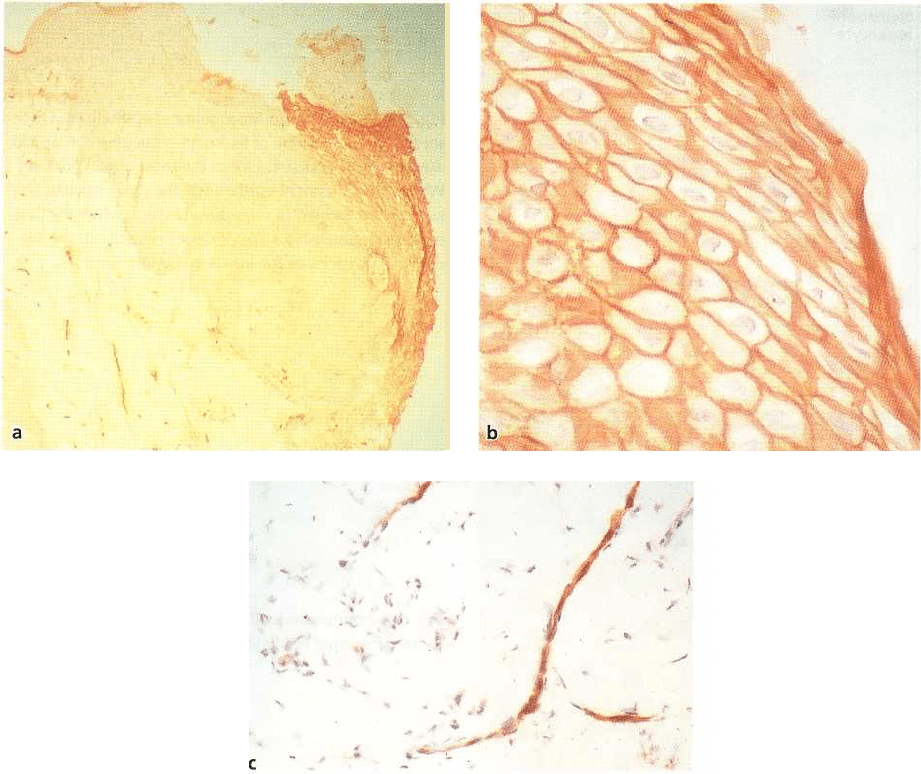
Fig. 5-4. Immunostained section showing neutrophils
in the junctional epithelium of healthy gingiva.
transudative fluid and plasma proteins arrive in the
gingival crevice region having left the vessels and
travelled through the tissues to create the gingival
crevicular fluid (GCF) (Egelberg 1967, Cimasoni 1983)
(Figs. 5-1 and 5-2). The infiltrate at this stage may
occupy as much as 5% of the connective tissue volume
and is composed of monocytes, macrophages, lym-
phocytes and neutrophils. These cells are found in the
junctional epithelium as well as in the connective
tissue of clinically healthy gingivae (Fig. 5-3). Neutro-
phils predominate in the crevice region and appear to
migrate continuously through the junctional epithe-
lium into the sulcus (Fig. 5-4). The recruitment of
leukocytes (predominantly PMNs) from the tissues to
the crevice is due both to the chemoattractant actions
of the host systems (interleukin-8, complement com-
ponent C5a, leukotriene B4 etc., see below) and prod-
ucts derived from the biofim (formyl methionyl leucyl
phenylalanine, lipopolysaccharide etc). With further
deposition of plaque and the development of overt
gingivitis, there is a marked increase in leukocytes
recruited to the area (Attstrom, 1971, Moughal et al.
1992). One additional effect of the inflammation
which encourages rapid accumulation of leukocytes
is the pro-inflammatory cytokine-mediated upregula-
tion of adhesion molecules on the endothelial cells.
This encourages leukocytes, particularly PMNs, in the
early stages to adhere to postcapillary venules and
begin migrating through the vessel and chemotacting
to the gingival crevice. This upregulation of adhesion
molecules (ICAM-1 and ELAM-1) occurs during "ex-
perimental gingivitis" (Loe et al. 1965) with a con-
comitant increase in leukocyte infiltration which cor-
responds with days of plaque accumulation (Kinane
et al. 1991, Moughal et al. 1992) (Fig. 5-5).
Clinically healthy gingiva appears to deal with
microbial challenges without progressing to a dis-
eased state, probably because of several defensive
factors which include:
1. Regular shedding of epithelial cells into the oral
cavity
2. Intact epithelial barrier
3. Positive fluid flow of the gingival crevice which
may remove non-attached microorganisms and
noxious products
154 • CHAPTER 5
Fig. 5-5. (a) ICAM-1 immunohistochemical staining of a gingival biopsy sample during an experimental gingivitis
study in humans after day 7. ICAM-1 positive blood vessels and junctional epithelium can be clearly seen.
(b) Higher magnification of Fig 5-5a showing the extensive junctional epithelium staining. (c) Higher magnification of
Fig 5-5a showing the ICAM-1 positive vessels within the connective tissue.
4. Antimicrobial effect of antibodies
5. Phagocytic function of neutrophils and macro-
phages
6. Detrimental effect of complement on the micro-
biota.
All of these factors may operate at the same time to
reduce the bacterial load and thus prevent an over-re-
sponse of the tissue defense systems which could
result in the formation of a lesion. The host-microbial
interplay which constitutes the clinically healthy situ-
ation must clearly change if gingivitis and periodon-
titis is to follow. Gingivitis will follow if there is suffi
cient plaque accumulation such that microbial prod-
ucts will initiate a substantive inflammatory response.
This response can be modified by hormones as in the
case of puberty or pregnancy (resulting in edematous
gingivitis) or by drugs such as phenytoin, cyclosporin
or nidefipine (which induce gingival overgrowth).
Gingivitis lesions are accompanied by more pro-
nounced loss of collagen albeit in discrete areas. The
gingivitis response will also initiate and perpetuate
immune responses to the oral microorganisms but the
level of this early response, particularly at the local
site, will be considerably less than the gross tissue
destruction and bone loss seen in more advanced
periodontitis lesions. Gingivitis may persist at sites for
many years without appreciable loss of periodontal
attachment, destruction of periodontal ligament or
evidence of bone loss. Clearly certain individuals (and
sites) go on to develop periodontitis from gingivitis
lesions whilst others remain resistant and merely ex-
hibit gingivitis responses to the accumulating plaque
microorganisms. Investigations of periodontal mani-
festations of systemic disease suggest that individuals
with obvious defects of the inflammatory system, e.g.
neutrophil depletion or dysfunction, may rapidly de-
velop severe periodontitis. In addition, there appears
to be a genetic predisposition to both aggressive and
chronic forms of periodontitis (Michalowicz et al.
2000, Hodge & Michalowicz 2001). There is an accu-
mulating body of evidence which suggests that the
host's immune response to periodontopathogens may
be quite different in those affected by chronic perio-
HOST-PARASITE INTERACTIONS IN PERIODONTAL DISEASE •
1
55
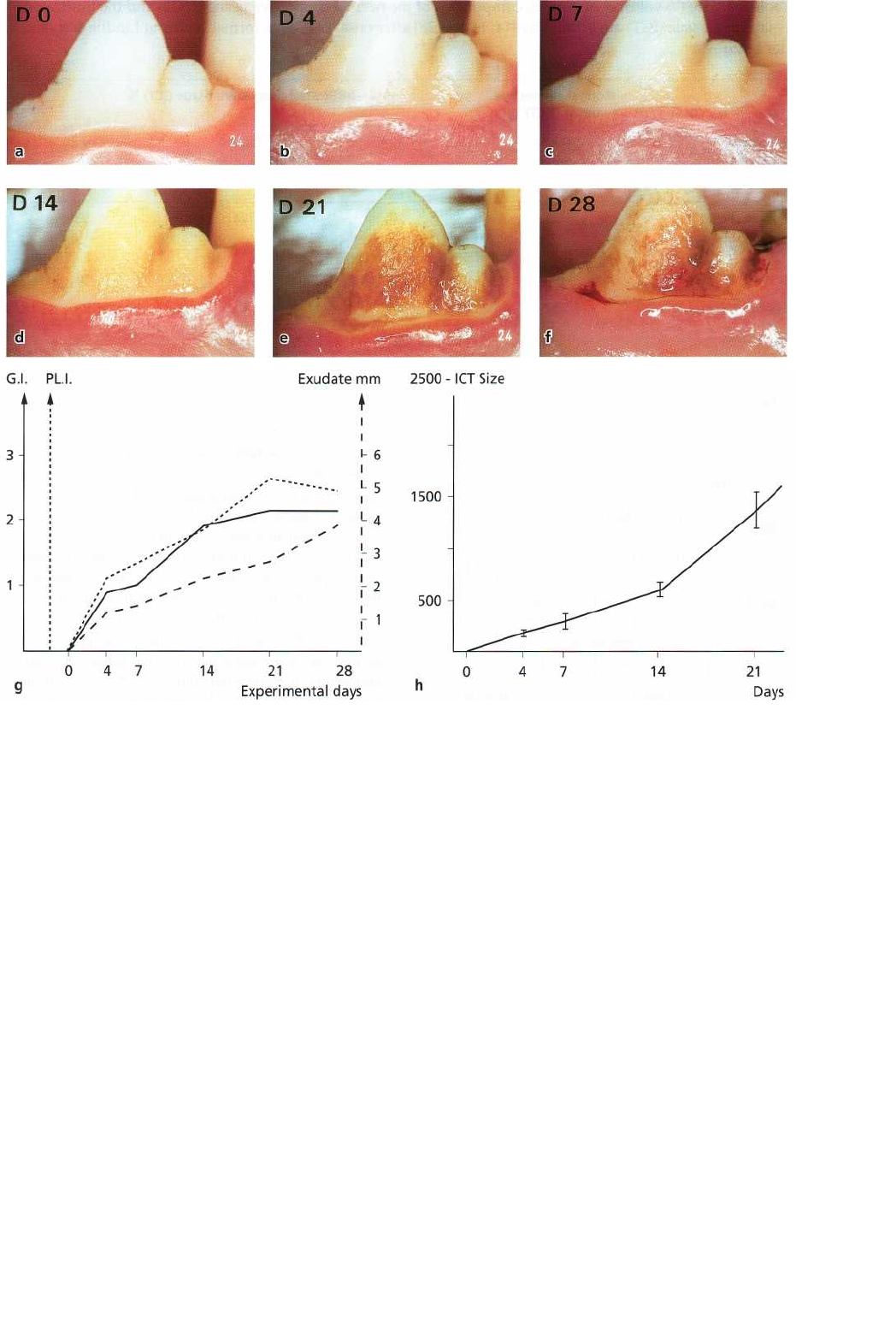
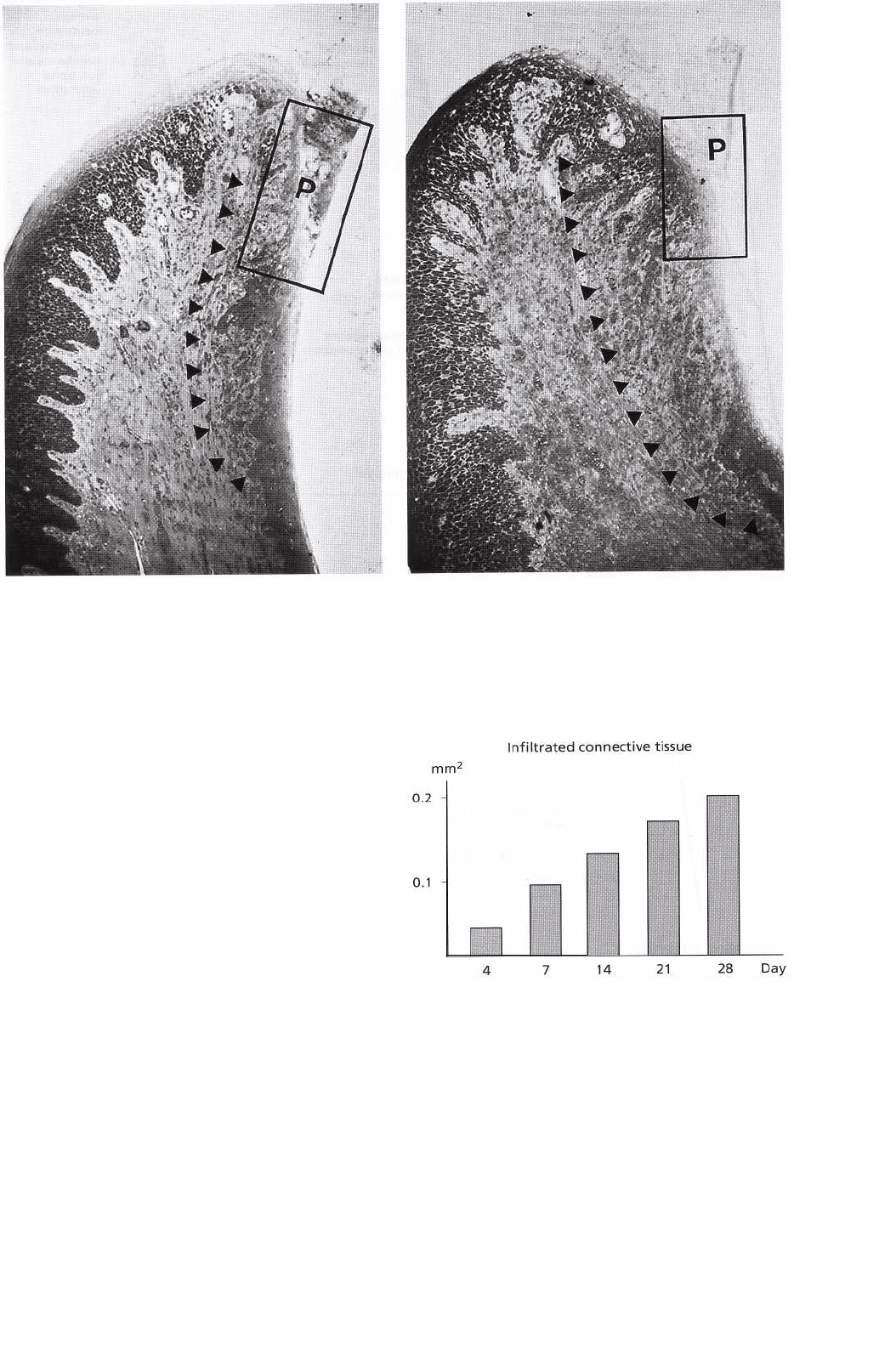
Fig. 5-6. Gingival alterations which occurred during a 28-day period of plaque accumulation and gingivitis devel-
opment in beagles. (a) Normal gingival. (b) Day 4. (c) Day 7. (d) Day 14. (e) Day 21. (f) Day 28 of undisturbed
plaque accumulation. Note the gradually developing plaque on the tooth surfaces and the inflammatory changes
in the gingiva. The vascular reaction is illustrated by a gradually increasing number of vessels in the gingival mar
-gin. (g) Gingival index (GI), plaque index (PLI) and gingival exudate alterations (exudate) that occurred during
the experimental gingivitis period. (h) In gingival biopsies obtained at various time intervals it can be seen that
the inflammatory cell infiltrate (ICT) in the gingiva gradually increased in size.
dontitis and those resistant to this disease, who would
not progress beyond gingivitis. There is also evidence
that "protective" antibodies increase following a
course of initial periodontal therapy, whereas those
individuals with a poor outcome following periodon-
tal therapy have antibodies which are less functional (
Mooney et al. 1995).
Initial, early, established and advanced
lesions
Introduction
Within 10-20 days of plaque accumulation, clinical
signs of gingivitis are established in most individuals,
although this varies greatly with some individuals
being intrinsically more resistant and others more
prone to overt gingivitis (Van der Weijden et al. 1993).
This gingivitis appears as gingival redness, swelling
and an increased tendency of the soft tissue to bleed on
gentle probing (Fig. 5-6). Even at this stage clinical
signs are reversible following removal of microbial
plaque by effective plaque control measures (Loe et al.
1965, Lindhe & Rylander 1975).
Histopathological features of gingival inflammation
The clinical changes may appear subtle in the early
stages of gingivitis but the underlying histopathologi-
cal changes are quite marked. Alterations in the vas-
cular network occur with many capillary beds being
opened up. Exudative fluid and proteins swell the
tissues and an influx of inflammatory cells in the
connective tissue occurs subjacent to the junctional
epithelium. The inflammatory cell infiltrate mainly
156 • CHAPTER 5
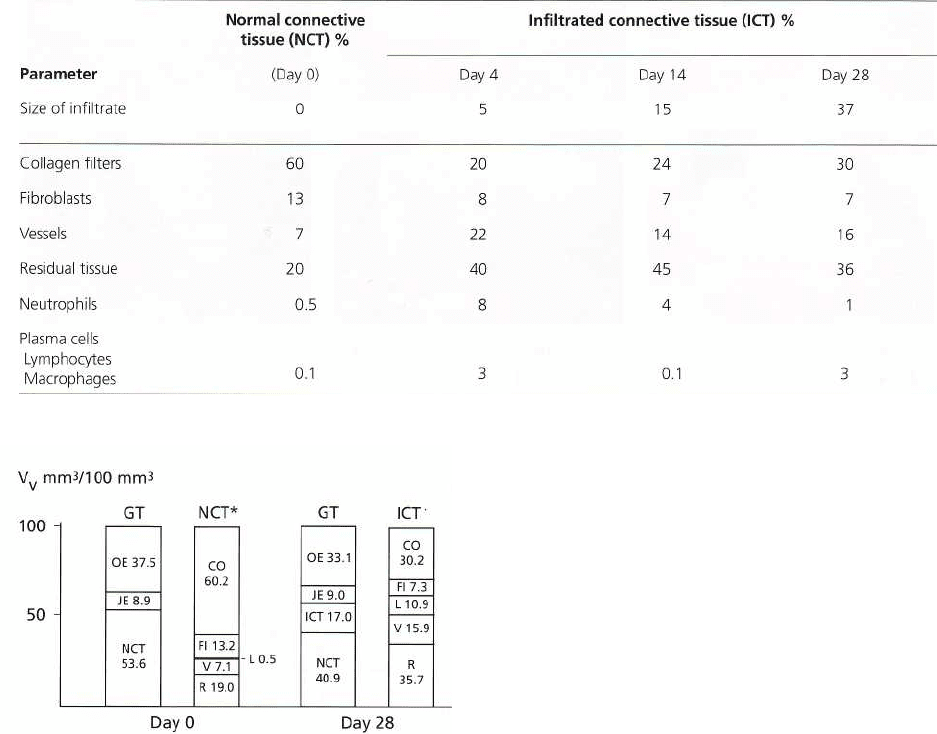
Table 5-1. Size (% volume) of various components of the normal connective tissue (NCT) and the infiltrated
connective tissue (ICT) at various days (4, 14 and 28) after onset of plaque formation (from Lindhe & Rylan-
der 1975)
comprises lymphocytes, macrophages and neutro-
phils. As the cellular infiltrate develops, the structural
and cellular composition of the tissues changes. An
experimental gingivitis study in dogs has compared
the cellular and structural composition of the affected
area before and during the development of gingivitis
over a period of 28 days (Lindhe & Rylander 1975).
Plaque was allowed to accumulate on the teeth of dogs
with initially normal gingiva, and biopsy samples
were taken at various times. The normal tissue (Day
0) is referred to below as non-infiltrated connective
tissue (NCT) and the altered area as the infiltrated
connective tissue (ICT) (Table 5-1).
At Day 0 of this dog experiment the normal gingival
unit has virtually no inflammatory cells (Fig. 5-7) and
is comprised of approximately 40-45% epithelium and
55-60% connective tissue. The NCT zone consists of
collagen (60%), fibroblasts (13%), vessels (7%) and
other tissue constituents, such as intercellular matrix
and nerves (20%). Following plaque accumulation,
neutrophils and mononuclear leukocytes readily mi-
Fig. 5-7. Composition of the gingiva (GT), non-infil-
trated (NCT) and infiltrated (ICT) gingival connective
tissue on day 0 (normal gingiva) and on day 28 of gin-
givitis in beagles. Note that the infiltrated connective
tissue portion amounts to 17% of the free gingival mar
-gin on day 28 and that the collagen content is reduced
from approximately 60% on day 0 to 30% on day 28 in
the area where the inflammatory infiltrate has become
established. Note also that in this area (on day 28) a re-
duction in fibroblast proportion has occurred, as well
as an increase of vessels and residual tissue. OE: oral
epithelium, JE: junctional epithelium, NCT: non-infil-
trated connective tissue, ICT: infiltrated connective tis-
sue, CO: collagen fibers, FI: fibroblasts, V: vascular
structures, L: leukocytes, R: residual tissue. (From
Lindhe & Rylander 1975)
grate to this area and the ICT begins to form and
increase in volume over the 28-day period. At this 28-
day interval the ICT is comprised of lymphocytes,
plasma cells and macrophages (Fig. 5-7) which adhere
to the collagen matrix and remain in the tissue,
whereas neutrophils continue to migrate into the gin-
gival sulcus. With the extensive influx of leukocytes, a
marked reduction in the amount of collagen and
fibroblasts occurs and the volume of residual tissue (
intercellular matrix, degraded collagen, exudate ma-
terial, degenerated or dead cells) and small blood
vessels increases.
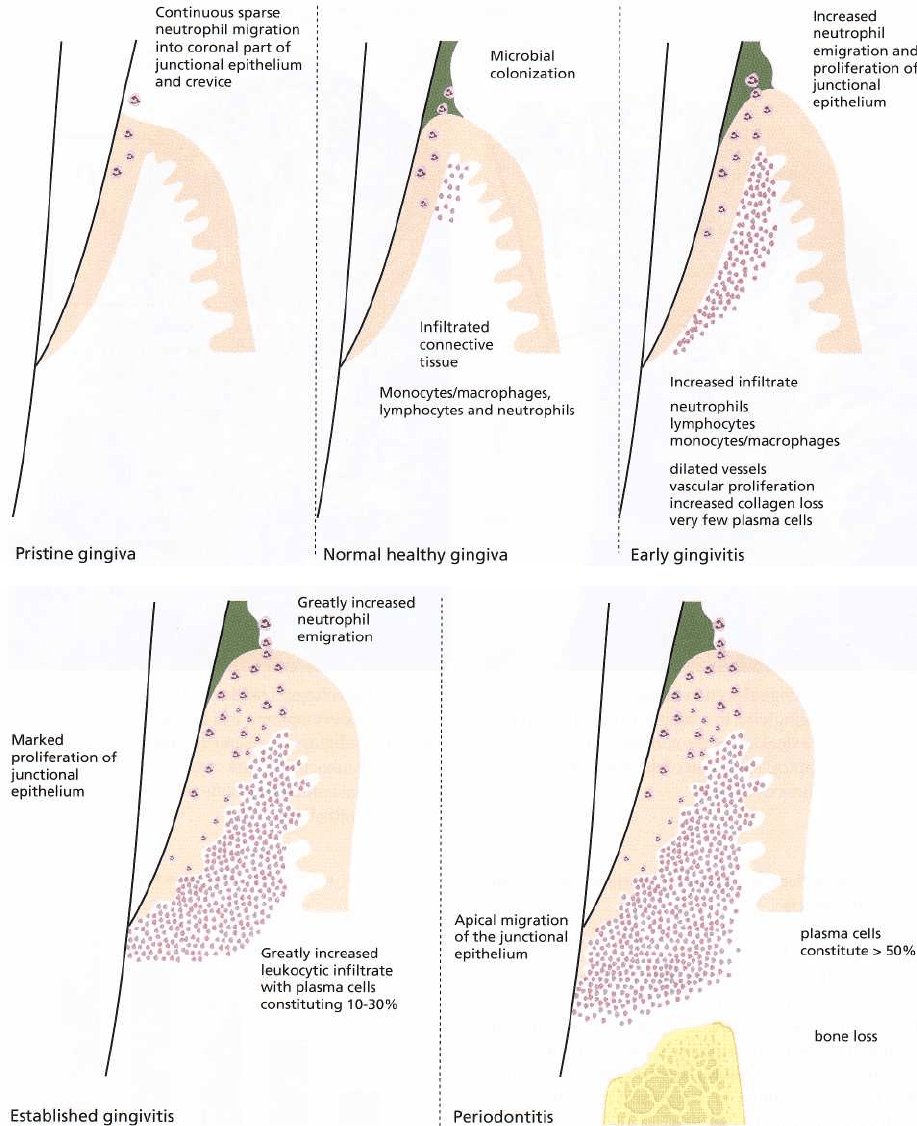
In 1976, Page and Schroeder classified the progres-
sion of gingival and periodontal inflammation on the
basis of the then available clinical and histopathologi-
cal evidence. They divided the progressing lesion into
four phases: initial, early, established and advanced stages
or lesions. The initial and early lesion descriptions
were thought to reflect the histopathology of clinically
early stages of gingivitis, while the established lesion
reflected the histopathology of more
HOST-PARASITE INTERACTIONS IN PERIODONTAL DISEASE • 157
"chronic" gingivitis. The description of the his-
topathology of the advanced lesion was considered to
reflect the progression of gingivitis to periodontitis.
The evidence on which these descriptions were based
was the prevailing information gleaned predomi-
nantly from animal biopsy material and some human
adolescent samples. Therefore the following account
by Page and Schroeder (1976) of lesion progression is
based very much on data from non-human experi-
ments.
The classical phases of "acute" and "chronic" in-
flammation are not easily applied in periodontal dis-
ease, probably because in most clinically healthy situ-
ations a lesion similar to an acute lesion occurs. Sub-
sequently, chronic inflammatory changes become su-
perimposed so that both acute and chronic elements
co-exist in early, established and advanced lesions. It
is important to repeat that in most clinically "normal"
human gingival biopsies a similar infiltrate can be
seen to that noted in the initial and early gingival
lesions of dogs. The Page and Schroeder system will
be utilized as a framework to outline the histopatho-
genesis of periodontal disease and modern conflicting
views will be outlined. A rational synthesis of opin-
ions will be attempted and a new classification based
on our current understanding of lesion progression
will be presented (Table 5-2).
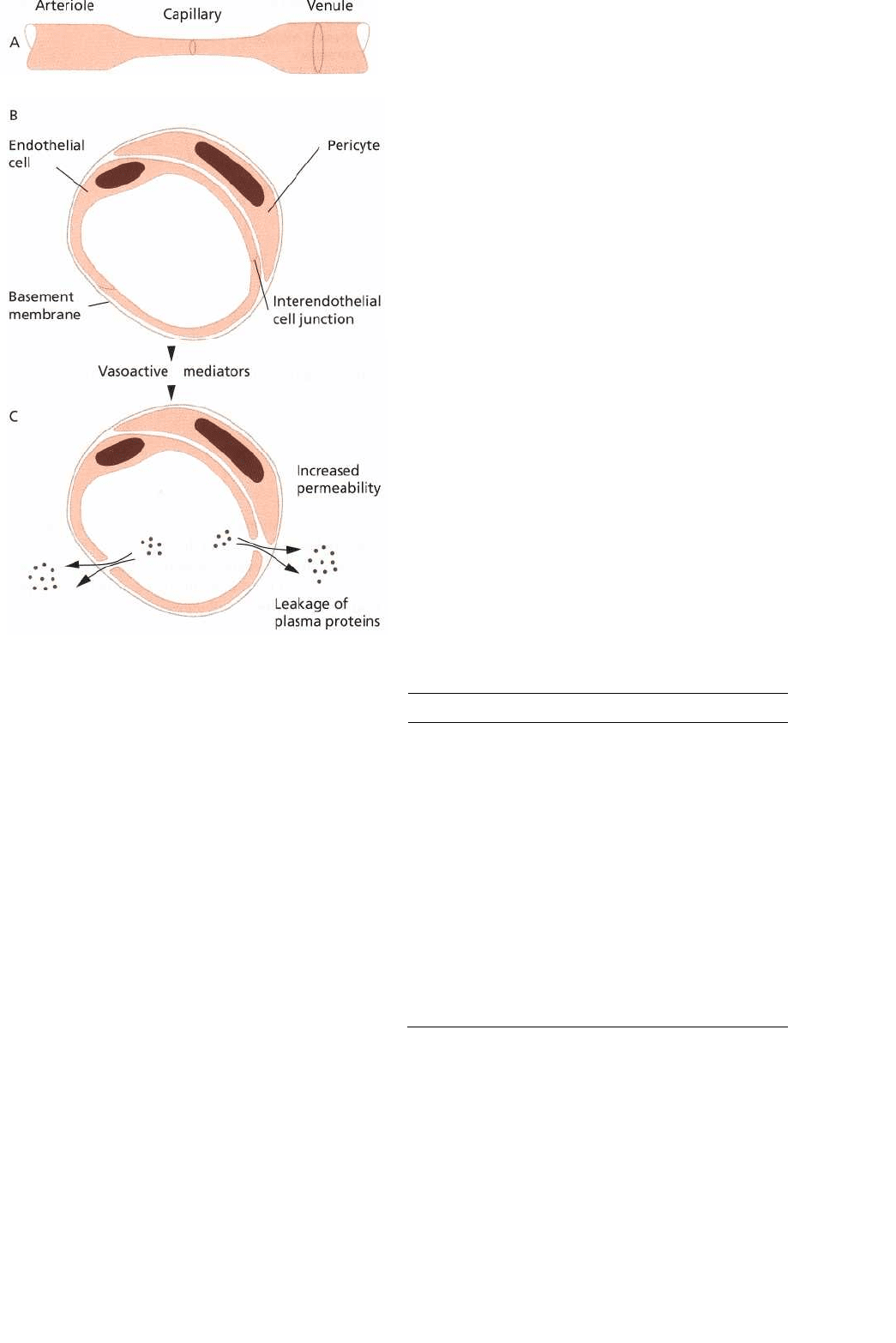
Fig. 5-8. Schematic illustrations depicting the terminal
vascular bed and the mechanisms of increased vascu-
lar permeability. Under normal conditions the terminal
vessels are freely permeable to small molecules, salt
and water. The intercellular junctions between the en-
dothelial cells are closed. Via the influence of vasoac-
tive mediators the endothelial cells become separated
and increased vascular permeability occurs. Large
molecules and plasma proteins leak into surrounding
tissue. A number of inflammatory mediators present in
plasma are activated when they enter the perivascular
tissue.
Clinical condition Histopathologic condition
Histologic perfection
Initial lesion of Page & Schroeder
Early lesion of Page & Schroeder (few
plasma cells)
Established lesion with no bone loss nor
apical epithelial migration (plasma cell
density between 10% and 30% of
leukocyte infiltrate)
Established lesion with bone loss and
apical epithelial migration from the
amelocemental junction (plasma cell
density > 50%)
The initial lesion
Inflammation quickly develops as plaque is deposited
on the tooth. Within 24 hours marked changes are
evident in the microvascular plexus beneath the junc-
tional epithelium as more blood is brought to the area.
Dilation of the arterioles, capillaries and venules of the
dentogingival plexus is evident histopathologically.
Hydrostatic pressure within the microcirculation in-
creases and intercellular gaps form between adjacent
Pristine gingiva
Normal health
gingiva
Early gingivitis
Established
gingivitis
Periodontitis
Table 5-2. A new classification is outlinec
158 • CHAPTER 5
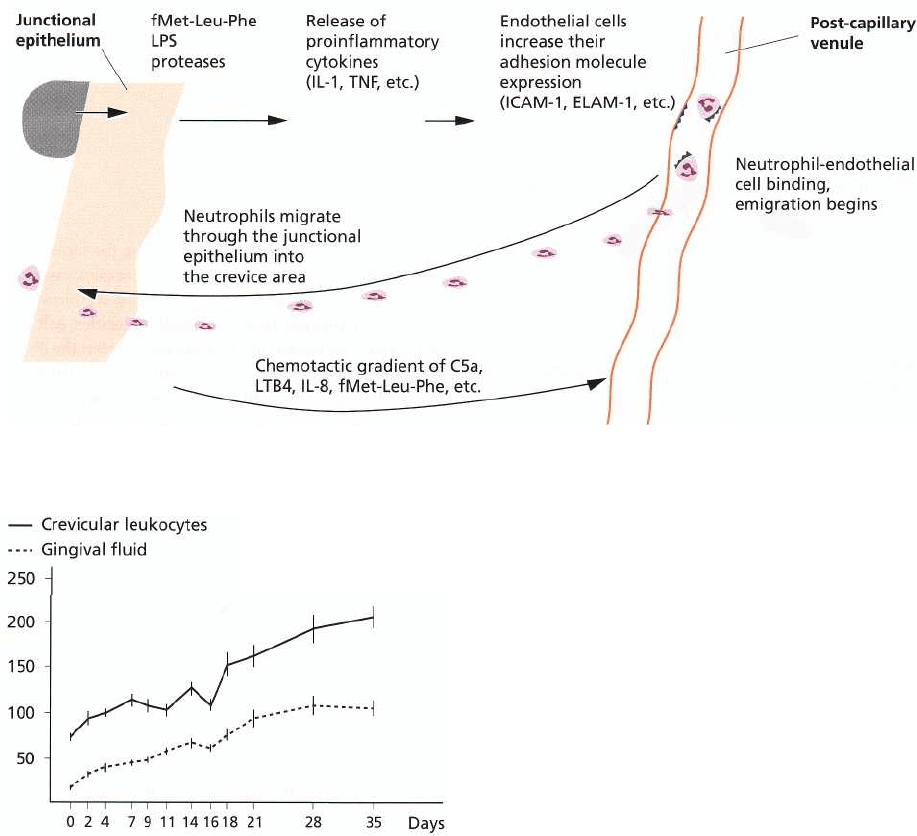
Fig. 5-9. Schematic illustration of the process whereby neutrophils are attracted into the junctional epithelium and
crevice region.
Fig. 5-10. Alterations in number of crevicular leuko-
cytes and in gingival fluid during a period of develop
ing gingivitis in beagles. Note the gradual increase
of leukocytes and fluid flow during the experimental
period. (From Attstrom & Egelberg 1970.)
capillary endothelial cells. An increase in the perme-
ability of the microvascular bed results, so that fluids
and proteins exude into the tissues (Fig. 5-8).
As the lesion enlarges, and gingival crevicular fluid
flow increases, noxious substances from microbes will
be diluted both in the tissue and the crevice. Bacteria
and their products may thus be flushed from the
sulcus. Plasma proteins escaping from the microcircu-
lation include defensive proteins such as antibodies,
complement and protease inhibitors and other macro-
molecules with numerous functions, which will be
discussed below. This gingival crevicular fluid (GCF)
can be readily sampled by placing filter strips at the
gingival margin to absorb the exudate. The volume of
the exudate is proportional to the severity of the gin-
gival inflammation present (Fig. 5-6). The absolute
amounts and the concentration of various plasma
proteins, tissue proteases, inhibitors and breakdown
products and leukocyte enzymes in the gingival sul-
cus have been studied extensively. GCF components
are considered as very useful markers of the inflam-
matory process and are currently being developed as
diagnostic markers of periodontal disease.
Simultaneously with these vascular alterations,
PMN cell migration from the dentogingival vascular
system is enhanced by the adhesion molecules, inter-
cellular adhesion molecule-1 (ICAM-1) and endothe-
lial leukocyte adhesion molecule-1 (ELAM-1) and
other adhesins. These molecules assist PMNs binding
to the post capillary venules and help the cells to leave
the blood vessel (Fig. 5-9). The leukocytes migrate up
a chemoattractant gradient to the crevice and are prob-
ably further assisted in their movement by the adhe-
sion molecules uniquely present on the junctional
epithelial cells (Fig. 5-5) (Moughal et al. 1992) and by
the presence of host and microbial chemotactic factors.
Lymphocytes may be retained in tissues on contact
with antigens, cytokines or adhesion molecules and
thus are not so readily lost through the junctional
epithelium and into oral cavity, as are PMNs. Most
lymphocytes have the ability to produce CD44 (CD =
cluster determinant) receptors on their surfaces,
which permit binding of the cell to the connective
tissue framework. This is consistent with the T and B
cell requirement to remain within the tissues and to
perform cell mediated and humoral immune func-
tions locally.
Probably within 2-4 days of plaque build-up the
HOST-PARASITE INTERACTIONS IN PERIODONTAL DISEASE •
1
59
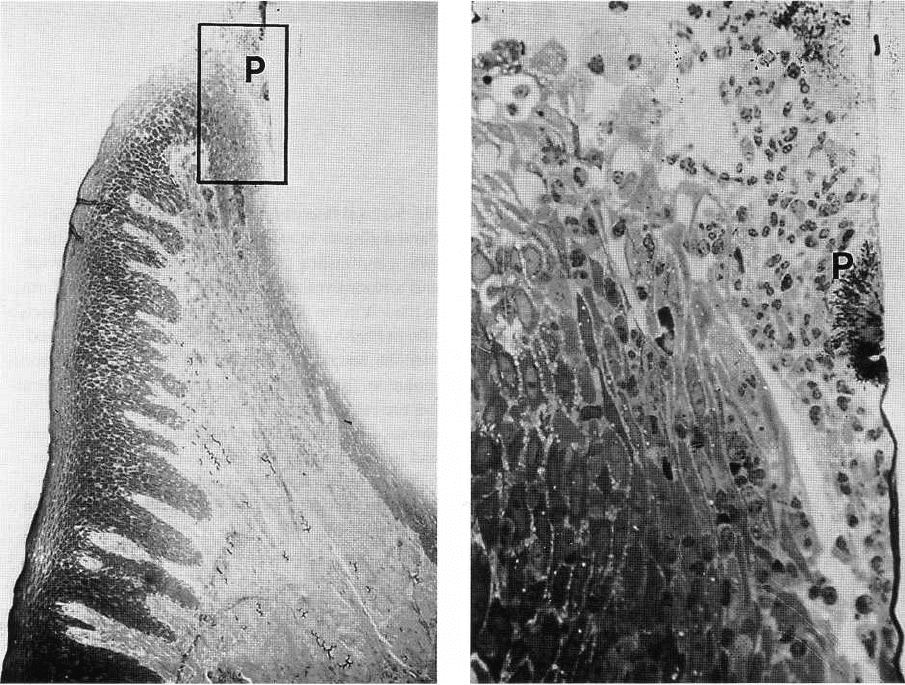
Fig. 5-11. Buccolingual section of the gingiva on day 4 of developing gingivitis in a beagle. Note plaque (P) in the
sulcus region and increased cellularity in the coronal part of the connective tissue below the junctional
epithelium. Note the presence of leukocytes in the coronal part of the junctional epithelium and at the surfaces of
the subgingival plaque.
cellular response is well established and is helped by
chemotactic substances originating from the plaque
microbiota as well as from host cells and secretions.
PMNs move through the connective tissue and the
majority seem to accumulate in the junctional epithe-
lium and gingival sulcus region (Figs 5-9 and 5-10).
The early lesion
The early gingival lesion occurs after approximately
one week of plaque accumulation (Fig. 5-11). Only an
approximation of the time required can be given as
marked subject variation occurs in humans although
this may well be less variable in animal models. The
variation seen amongst humans could be due to dif-
ferences in plaque accumulation, both at the site and
subject level, or to differences between individuals in
features such as hormonal levels. Histologically the
vessels below the junctional epithelium remain di-
lated, but their numbers increase due to the opening
up of previously inactive capillary beds (compare Fig.
5-1 and 5-12). The course, size and quantity of mi-
crovasculature units are reflected in the clinical ap-
pearance of the gingival margin during this phase (
Egelberg 1967, Lindhe & Rylander 1975).
Lymphocytes and PMNs are the predominant infil-
trating leukocytes at this stage and very few plasma
cells are noted within the lesion (Listgarten & Elle-
gaard 1973, Payne et al. 1975, Seymour et al. 1983,
Brecx et al. 1987). The inflammatory cell infiltrate may
at this stage comprise as much as 15% of the connec-
tive tissue volume. Within the lesion fibroblasts de-
generate. This probably occurs by apoptosis and
serves to remove fibroblasts from the area, thus per-
mitting more leukocyte infiltration (Page & Schroeder
1976, Takahashi et al. 1995). Similarly collagen de-
struction occurs in the infiltrated area and is necessary
in order that the tissues can be pushed apart to accom-
modate the infiltrating cells and thus could be consid-
ered as a space creating process. Inflammatory
changes are detectable clinically at this stage and near-
ing the end of the second week of plaque accumula-
tion, a subgingivally located biofilm can be found.
The basal cells of the junctional and sulcular epithe-
lium have now proliferated. This represents an at-
tempt by the body to enhance the innate barrier to
plaque (Fig. 5-13). Epithelial rete pegs can be seen
invading the coronal portion of the lesion (Schroeder
1970, Schroeder et al. 1973).
The duration of the early lesion in humans has not
been determined. The early lesion may persist for
much longer than previously thought and the vari-
ability in time required to produce an established
160 • CHAPTER 5
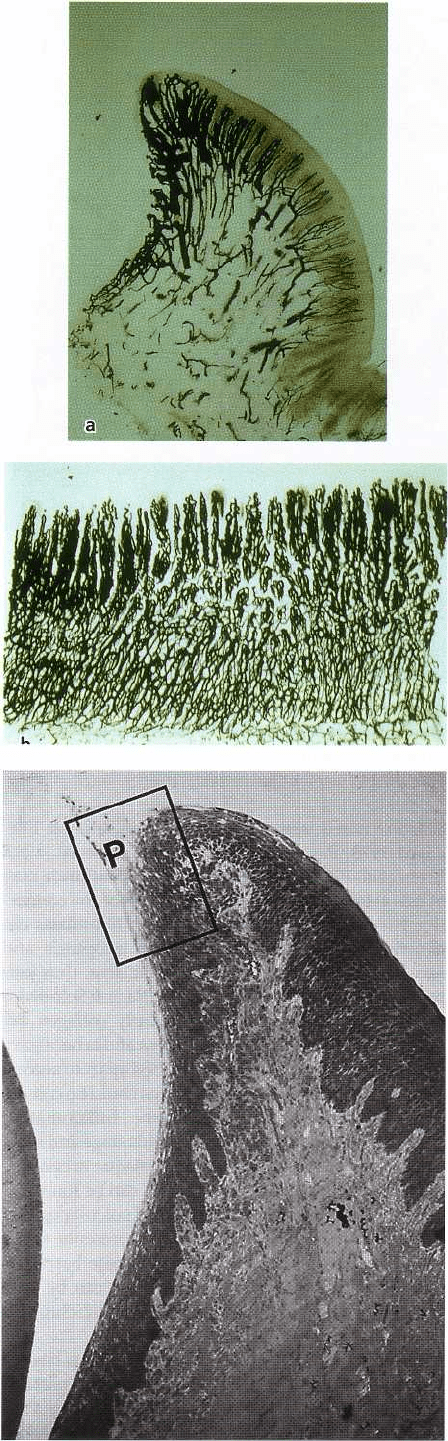
Fig. 5-12. (a) Buccolingual section of chronically in-
flamed gingiva in a dog. The vessels have been filled
with a contrasting carbon suspension. Note the wide
and tortuous vessels below the junctional epithelium
to the left in the illustration. Compare with the vascula-
ture in healthy gingiva in Fig. 5-10. The pronounced
vascular reaction in this area is a result of plaque accu-
mulation. (b) Mesiodistal section of a gingiva illustrat-
ing the vessels below the junctional epithelium of
chronically inflamed gingiva. Note vascular dilation
and proliferation at the level of the gingival margin (
GM). Note also that vascular proliferation has oc-
curred in the apical part of the vascular plexus (from
Egelberg 1967).
Fig. 5-13. Buccolingual section of the gingiva on day 7
of developing gingivitis in a beagle. Note the subgingi-
val extension of plaque (P), as well as the increased
number of inflammatory cells in the connective tissue
below the dentogingival epithelium.
HOST-PARASITE INTERACTIONS IN PERIODONTAL DISEASE • 161
Fig. 5-14. Buccolingual section of the gingiva on day 21
of developing gingivitis in a beagle. Compare with Fig.
5-15. Note the extension of the subgingival plaque (P)
as well as the apical extension of the infiltrate (the le-
sion) in the connective tissue.
Fig. 5-15. Buccolingual section of the gingiva on day 28
of gingivitis development in a beagle. Note the exten-
sion of the subgingival plaque (P) and the increased
number of leukocytes in the connective tissue below
the junctional epithelium. Note rete pegs in the den-
togingival epithelium.
lesion may reflect susceptibility variance within and
between subjects.
The established lesion
Generally there is a further enhancement of the in-
flammatory state as exposure to plaque continues.
There is increased fluid exudation and leukocyte mi-
gration into the tissues and the gingival crevice. Clini-
cally this lesion will exhibit more edematous swelling
than the "early gingivitis" lesion and could be consid-
ered as "established gingivitis".
The established lesion as defined by Page and
Schroeder is one dominated by plasma cells. This
conclusion was based mainly on data from animal
experiments. However, Brecx et al. (1988) demon-
strated that even following 6 months of oral hygiene
neglect, the plasma cell fraction in human biopsies
comprised only 10% of the cellular infiltrate and was
clearly not the dominant cell type. Thus, the human
established lesion apparently requires much more time
to "mature" than its animal counterparts.
In the established lesion described by Page and
Schroeder (1976), plasma cells are seen situated pri-
marily in the coronal connective tissues as well as
Fig. 5-16. Diagram showing the increase in size of the
infiltrated connective tissue during the development of
gingivitis in beagles (from Mattsson & Attstrom 1979)
.
around vessels. Collagen loss continues in both lateral
and apical directions as the inflammatory cell infil-
trate expands, resulting in collagen depleted spaces
extending deeper into the tissues which are then avail-
able for leukocytic infiltration (Figs. 5-14, 5-15, 5-16).
During this time the dentogingival epithelium contin-
162 • CHAPTER 5
Fig. 5-17. Schematic illustration of the changes in the gingival tissues during the development of gingivitis and
periodontitis. The most significant differences are in the extent and composition of the inflammatory infiltrate and
the epithelial proliferation in gingivitis, and the apical migration of epithelium and bone loss seen in periodontitis
lesions.
ues to proliferate and the rete pegs extend deeper into
the connective tissue in an attempt to maintain epi-
thelial integrity and a barrier to microbial entry. The
junctional epithelium is changed and is no longer
closely attached to the tooth surface. The pocket epi-
thelium that now has formed has a heavy leukocyte
infiltrate, predominantly of PMNs which eventually
migrate across the epithelium into the gingival pocket.
In comparison to the original junctional epithelium,
the pocket epithelium is more permeable to the pas-
sage of substances into and out of the underlying
connective tissues and may in places be temporarily
ulcerated. Fig. 5-17 schematically illustrates the altera
tions which occur in the epithelium and the connec-
